Understanding Dysphagia

by Jane Hurd, MPA, Jeri Logemann, Ph.D., Nancy L. Matthews, MA, Charles A. Stewart, M.D., Diane J. Aschman, MS
At the age of 78, Maxine was a poster girl for an active senior lifestyle. She loved being the unofficial social director of her assisted living community in the Texas Hill Country, organizing shopping trips to San Antonio and calling the numbers at the daily bingo game. Physically, Maxine was in great shape. She took a brisk walk every morning and had a regular annual physical exam. Her only chronic health problem was mild Parkinson’s, which she controls with daily medication.
Since Maxine especially enjoyed sitting with her special friends at dinner, she was very concerned when she began to experience prolonged coughing fits at the table. At first she thought the problem might be simply trying to talk, eat, and breathe at the same time – so she decided to listen more and speak less. Things got better for a while, though her friends did notice how quiet and subdued she seemed.
Eventually, Maxine began to skip going to dinner and ate in her room instead. She also began to have difficulty swallowing her medication and vitamins. Sometimes she needed a whole glass of water to get them down. Worried, she began to have trouble going to sleep, which made her look tired. This change was very apparent to Maxine’s daughter when she came to visit from out-of-state. Maxine had always been so upbeat and positive. Now, for the first time, she seemed confused and depressed.
Dysphagia:
What we don’t know can hurt us.
Dysphagia is the medical term for difficulty or inability to swallow. Although it’s rarely talked about, dysphagia can have an immediate negative impact on quality of life. Eating, after all, is a pleasurable group activity. A good meal satisfies more than just the appetite. This may be especially true for residents of independent or assisted living communities, for whom mealtimes are a highlight of the day. Beyond the social issues, dysphagia can also have serious health-related consequences, including malnutrition, dehydration, and aspiration pneumonia.
Yet difficulties in swallowing are not a natural result of aging. They are treatable and preventable, with recognition of the problem as the first step. However, there is evidence that dysphagia is often undiagnosed or untreated: a recent study in Los Angeles County found incidence of swallowing issues in approximately 11 percent of seniors in assisted or independent living facilities. Administrators in these facilities confirm that residents’ swallowing disorders are often unnoticed until the condition has become fully established. At that point, a feeding tube may become necessary. As a result, the resident may need to be transferred to a skilled care environment where appropriate support can be provided. Ignored or unidentified, dysphagia can lead to a basic loss of independence and self-sufficiency.
Recognition, Education, Control
Dysphagia has a variety of causes and can manifest in a variety of ways. To identify the problem, the right questions need to be asked in easily understood language. It may also be necessary to eliminate some common myths and misunderstandings. Education, therefore, is a key element in bringing dysphagia under control. This can begin with an understanding of the swallowing process itself.
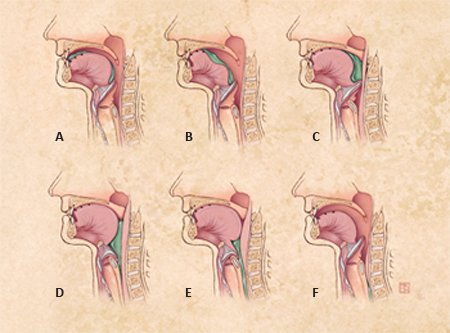
In Picture A, a morsel of food has been chewed and is ready to enter the throat.
The food then pushed toward the back part of the mouth, against the muscles of the pharyngeal wall as seen in Pictures B and C.
In Pictures D and E, the airway lifts and closes off when the soft pallet closes, protecting the entrance to the nose. Then the entrance to the esophagus opens, allowing food to bypass the airway and enter the esophagus.
Finally, in Picture F the food passes down the esophagus. The airways reopen to allow continued breathing.
When this sequence is disrupted at any point, dysphagia can result. Because individuals may seek to avoid the embarrassment of coughing or choking during meals, they isolate themselves to the extent that early signs go unrecognized. In making the diagnosis, it’s important to be aware of conditions such as Parkinson’s or gastro-esophageal reflux (GERD), which can heighten vulnerability. Dysphagia may also arise as a side effect of medication often used for arthritis, Parkinson’s disease, depression and other common conditions.
While it’s important to educate care providers about dysphagia, it’s also crucial that seniors themselves learn to recognize symptoms and seek treatment. For this to happen, a number of longstanding barriers need to be overcome:
Many people with symptoms of dysphagia fail to report them to physicians or caregivers, often to avoid embarrassment. They may fear loss of independence, or reduced enjoyment from meals.
In its early stages, individuals may be unaware of the signs and symptoms of dysphagia, or may choose to ignore them.
Dysphagia may be seen as a “normal” part of the aging process.A person may be unaware of the mechanics of swallowing and of safe swallowing strategies.
Individuals may not realize that there is a clinical specialty dealing with swallowing problems, and that help is readily available.
Most importantly, people may see swallowing issues as insignificant, and remain unaware of the potential consequences.
The Happy Ending
With her daughter’s help, Maxine’s story began to turn around. Her daughter arranged for Maxine to visit her primary care physician, who referred Maxine to a speech and language pathologist in the outpatient department of a local medical center. Janice, the SLP, asked Maxine about her medical history and her current medical status. Then Janice performed a “tabletop clinical evaluation,” examining Maxine’s facial and throat muscle strength, and watching her swallow measured amounts of water, pudding, and Lorna Doone cookies. This wasn’t at all an unpleasant or threatening experience. In fact, Maxine began to feel better right away because Janice assured her that there were definitely ways to improve her swallowing even if she were found to have a dysphagia.
Janice recommended that Maxine’s doctor refer her to the medical center’s radiology department for an x-ray procedure called modified barium swallow, or MBS. Maxine was impressed by the fact that the radiologist would watch her swallowing in real time and could see exactly where she was having a problem – but she was also apprehensive about having to swallow the small amount of barium. But it turned out to be no problem, and no more uncomfortable than the “tabletop clinical evaluation,” and Janice was with her the whole time.
As it turned out, Maxine did have dysphagia, probably brought on by her Parkinson’s. But by identifying the problem early, she was able to improve her swallowing and go back to her busy social life. Janice taught her exercises to improve the strength, range of motion, speed, and coordination of her swallowing process. She also learned which foods are most likely to cause choking. These can vary from one person to another. In Maxine’s case they included anything with vinegar and foods such as watermelon that have both solid and liquid consistency. While she will always need to be careful, Maxine is back to her cheerful self, presiding over meals and bingo games.