One Last Visit to See My Patient
By Danielle
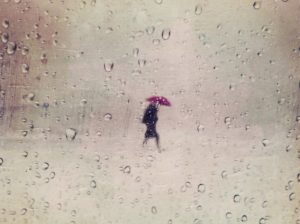
The rain was coming down in torrents and my shoes were not up to the job. Nevertheless, I pressed forward along the soggy blocks. My 91-year-old patient and I had been together for some 20 years — honestly I’d lost count — so this was the least I could do.
Fibrotic lungs and a weak heart set in a 4-foot-5 frame of osteoporotic bones would not seem the stuff of stamina, but until recently, she was still making the grueling 20-hour plane trip back to the Philippines every autumn. She had bounced back from several stays in the I.C.U. even well into her 80s.
My patient’s daughters took exquisite care of her. It was clear that every medical issue was rigorously attended to, but it was also clear that she was abundantly steeped in love. It’s hard for me to remember a time when she wasn’t smiling.
Even as her body and mind grew more frail, she was unfailingly cheerful. At one visit to our clinic, I asked about her hobbies. She told me that she liked to sing along with hymns on the stereo. She sang one for me, easily the most mellifluous sound ever to traverse our hospital’s halls.
Eighteen months earlier, I had raised the issue of hospice care. The family was hesitant — they were very private people and didn’t want anyone in their home. But I suspected that they were also put off by their associations with hospice. For most people, the word hospice means “game over.”
But hospice should actually be thought of as “game on” — now it’s time to really start taking care of the patient. And contrary to the assumption that hospice equals death, data show that early referral to hospice actually improves life expectancy.
My patient and her family agreed to give hospice a try. Within weeks, they were singing its praises. The hospice nurse visited weekly and whenever a clinical situation arose — a fever, pain, trouble breathing, a fall, — the nurse texted me and we could quickly figure out what needed to be done, and how to do it with the least hassle for the patient. Even though we weren’t pursuing “curative therapy” — her cardiac and respiratory disease were grave and irreversible — we were able to put out the little fires before they became big fires. The goal was always maximizing comfort.
In some ways, hospice care struck me as the original “concierge medicine,” where a whole team of players dedicated itself to the patient’s every need. This was the closest we could get to ideal medical care.
It didn’t escape me, though, that this level of care could only be feasible for a handful of patients. If every one of my hundreds of patients had my cellphone number and texted every time something came up, the system would collapse under its own weight.
Still, I was intensely grateful that this patient remained comfortable, happy, pain-free and able to remain in her home with her loving family. Just as the data predicted, she was living far longer than any of us would have expected, given her congestive heart failure and her severe respiratory disease. It was now 18 months since we started the hospice care.
The paradox is that a patient can qualify for hospice care only if he or she has a life expectancy of six months or less, if the disease runs its normal course. My patient certainly fit that definition, but as we focused intensely on making her more comfortable, she was living longer. Every six months I recertified that my patient indeed had end-stage cardiac and respiratory disease. And although she was clearly frailer at each certification, she remained comfortable and pain-free.
Most patients, sadly, get referred to hospice only in the very last days or weeks of their illness, which explains the misperception that “nothing” is done for the patient other than fluff the pillows on the way to death. Even for patients with end-stage cancer, the earlier they are referred to palliative care (care focused on patient comfort), the longer they usually live.
These thoughts circled in my head as I slogged through the torrential rain toward my patient’s home. I’d asked her daughter if maybe we could reschedule for the next day, when it would be less monsoon-like. “I think you should probably come today,” her daughter replied. Her voice was straightforward and unhurried, but as soon as she said that I angled my umbrella into the downpour and didn’t lift it until I arrived at her building, 20 sopping blocks later.
Their apartment was brimming with ferns, vines and succulents. It was almost as if they’d recreated the jungle of their home country in the concrete of New York City. In the midst of this verdant lair, my patient reclined comfortably on the couch, her face radiating warmth and welcome amid the greenery and medical equipment surrounding her. She gave me a big hug and invited me onto the couch next to her. A breathing mask from a nearby BiPAP machine covered her mouth and nose, but she could still talk. It was obvious how proud she was of her two daughters who sat nearby.
Sitting there, it dawned on me that my patient had won the lottery. She’d lived a long and happy life, with a loving extended family in two countries. Her final days were being spent on her own couch, among her plants and family, her favorite TV shows and music.
After 45 minutes visiting, I kissed her goodbye and shared hugs with the daughters. I headed back out into the rain, nursing a sadness and a relief at the same time.
That evening her daughter called me. Her mother had died peacefully on the couch, just hours after I’d left. The moment froze as the solemnity of her words sank in. Yes, we’d been expecting this for more than a year, but now it had actually happened. Even as we spoke, the hospice team was taking care of the logistics so that the family — and I — could focus on the emotions of the moment, and not the overwhelming details.
“I think she needed one more visit from her doctor before she could go,” her daughter said. We both exhaled long sighs — we’d been taking care of her mother together for two decades and now she had quietly bowed out. Once again, I felt the strange churning of melancholy and joy.
We rarely think of death as a moment of joy, but this was certainly one. Even in my sadness, I could feel the warmth of happiness for my patient that she’d been able to end her life cradled in love and comfort. She certainly did win the lottery.
I hope we all have that chance.

